
2023 American Heart Association and American Academy of Pediatrics Focused Update on Neonatal Resuscitation: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care
Nicole K. Yamada, MD, MS; Edgardo Szyld, MD, MSc, Co-Chair; Marya L. Strand, MD, MS; Emer Finan, MB, MEd; Jessica L. Illuzzi, MD, MS; Beena D. Kamath-Rayne, MD, MPH; Vishal S. Kapadia, MD, MSCS; Susan Niermeyer, MD, MPH; Georg M. Schmölzer, MD, PhD; Amanda Williams, RN, CNS, MSN; Gary M. Weiner, MD; Myra H. Wyckoff, MD; Henry C. Lee, MD, Co-Chair; on behalf of the American Heart Association and American Academy of Pediatrics
DOI: 10.1542/peds.2023-065030
Journal: Pediatrics
Article Type: Special Article
Citation: Yamada NK, Szyld E, Strand ML, et al. 2023 American Heart Association and American Academy of Pediatrics Focused Update on Neonatal Resuscitation: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics. 2023; doi: 10.1542/peds.2023-065030
This is a prepublication version of an article that has undergone peer review and been accepted for publication but is not the final version of record. The journal is providing an early version of this article to expedite access to this information. The American Academy of Pediatrics, the editors, and authors are not responsible for inac- curate information and data described in this version.
©2023 American Academy of Pediatrics and American Heart Association Inc
Prepublication Release
AHA/AAP FOCUSED UPDATE
2023 American Heart Association and American Academy of Pediatrics Focused Update on Neonatal Resuscitation: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care
Nicole K. Yamada, MD, MS; Edgardo Szyld, MD, MSc, Co-Chair; Marya L. Strand, MD, MS; Emer Finan, MB, MEd; Jessica L. Illuzzi, MD, MS; Beena D. Kamath-Rayne, MD, MPH; Vishal S. Kapadia, MD, MSCS; Susan Niermeyer, MD, MPH; Georg M. Schmölzer, MD, PhD; Amanda Williams, RN, CNS, MSN; Gary M. Weiner, MD; Myra H. Wyckoff, MD; Henry C. Lee, MD, Co-Chair; on behalf of the American Heart Association and American Academy of Pediatrics
ABSTRACT: This 2023 focused update to the neonatal resuscitation guidelines is based on 4 systematic reviews recently completed under the direction of the International Liaison Committee on Resuscitation Neonatal Life Support Task Force. Systematic reviewers and content experts from this task force performed comprehensive reviews of the scientific literature on umbilical cord management in preterm, late preterm, and term newborn infants, and the optimal devices and interfaces used for administering positive-pressure ventilation during resuscitation of newborn infants. These recommendations provide new guidance on the use of intact umbilical cord milking, device selection for administering positive-pressure ventilation, and an additional primary interface for administering positive-pressure ventilation.
Key Words: AHA Scientific Statements ■ infant ■ infant, newborn ■ intermittent positive-pressure ventilation ■ laryngeal masks
- respiration, artificial ■ umbilical cord clamping ■ umbilical cord milking
TOP 10 TAKE-HOME MESSAGES FOR NEONATAL RESUSCITATION
- For term and late preterm newborn infants ≥34 weeks’ gestation who do not require resuscitation, delayed cord clamping (≥30 seconds) can be beneficial compared with early cord clamping (<30 seconds).
- For term and late preterm newborn infants ≥34 weeks’ gestation who do not require resuscitation, intact cord milking is not known to be beneficial compared with delayed cord clamping (≥30 seconds).
- For nonvigorous term and late preterm newborn infants (35–42 weeks’ gestation), intact cord milking may be reasonable compared with early cord clamping (<30 seconds).
- For preterm newborn infants <34 weeks’ gestation who do not require resuscitation, delaying cord clamping (≥30 seconds) can be beneficial compared with early cord clamping (<30 seconds).
- For preterm newborn infants between 28 and 34 weeks’ gestation who do not require resuscitation and in whom
delayed cord clamping cannot be performed, intact cord milking may be reasonable.
- For preterm newborn infants <28 weeks’ gestation, intact cord milking is not recommended.
- Effective positive-pressure ventilation is the priority in newborn infants who need support after birth.
- Using a T-piece resuscitator to deliver positive-pressure ventilation is preferred to the use of a self-inflating bag.
- Because both T-piece resuscitators and flow-inflating bags require a compressed gas source to function, a
self-inflating bag should be available as a backup in the event of compressed gas failure when using either of these
©2023 American Academy of Pediatrics and American Heart Association Inc
devices.
- Use of a supraglottic airway may be considered as the primary interface to administer positive-
pressure ventilation instead of a face mask for newborn infants delivered at ≥34 0/7 weeks’ gestation.
Abbreviations
| AAP | American Academy of Pediatrics |
| AHA | American Heart Association |
| COR | class of recommendation |
| DCC | delayed cord clamping |
| ILCOR | International Liaison Committee on Resuscitation |
| LOE | level of evidence |
| PPV | positive-pressure ventilation |
| RCT | randomized controlled trial |
- INTRODUCTION
Scope of the Guidelines
These guidelines are designed for North American health care practitioners caring for newborn infants who are looking for an up-to-date summary for clinical care, and for those who are seeking more in-depth information on these topics in resuscitation science and the gaps in current knowledge. This focused update is based on the systematic reviews of umbilical cord management in term and late preterm infants1 and preterm infants,2 and the devices and interfaces for administering positive-pressure ventilation (PPV).3,4 The findings of those systematic reviews are also reported in the “2021 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations”5 and the “2022 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations”6 from the International Liaison Committee on Resuscitation (ILCOR). The guidelines contained in this document serve as an update on these topics from the “2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care”7 and “Neonatal Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations” from the ILCOR Neonatal Life Support Task Force.8
Organization of the Writing Group
The Neonatal Life Support writing group includes neonatal physicians and nurses with backgrounds in clinical medicine, education, research, and public health. Volunteers with recognized expertise in neonatal resuscitation are nominated by the writing group co-chairs. Writing group members were selected by the American Heart Association (AHA) Emergency
©2023 American Academy of Pediatrics and American Heart Association Inc
Cardiovascular Care Science Subcommittee and the American Academy of Pediatrics (AAP) Executive Board and then
approved by the AHA Manuscript Oversight Committee.
The AHA and the AAP have rigorous conflict of interest policies and procedures to minimize the risk of bias or improper influence during the development of guidelines. Before their appointment, writing group members disclosed all relevant commercial relationships and other potential (including intellectual) conflicts. Writing group members whose research led to changes in guidelines were required to declare those conflicts during discussions and abstain from voting on those specific recommendations. These procedures are described more fully in “Part 2: Evidence Evaluation and Guidelines Development” of the 2020 guidelines.9
Appendix 1 of this document lists disclosure information and the writing group members’ relevant relationships with
industry.
Methodology and Evidence Review
Updated AHA/AAP guidelines for cardiopulmonary resuscitation and emergency cardiovascular care are developed in concert with ILCOR’s continuous evaluation of new resuscitation science.9 This 2023 focused update is based on 4 systematic reviews completed by the ILCOR Neonatal Life Support Task Force, which reviewed the science on umbilical cord management in preterm, late preterm, and term newborn infants1,2 and on devices and interfaces for administering PPV for newborn infants.3,4 The ILCOR Neonatal Life Support Task Force used the findings of these systematic reviews to draft treatment recommendations, which were posted online for public comment. The final wording has been published in the Consensus on Science With Treatment Recommendations summary documents from 2021 and 2022.5,6 Full details on the ILCOR systematic review process can be found in the 2022 publication.6 For this 2023 focused update, the Neonatal Life Support writing group analyzed and discussed the systematic reviews, carefully considered the treatment recommendations drafted by the ILCOR Neonatal Life Support Task Force, and incorporated new data published since the systematic reviews were completed. Guideline recommendations were drafted by designated writing group members and then reviewed and refined by all writing group members during regular meetings. The final recommendation wording was reviewed and approved by all writing group members.
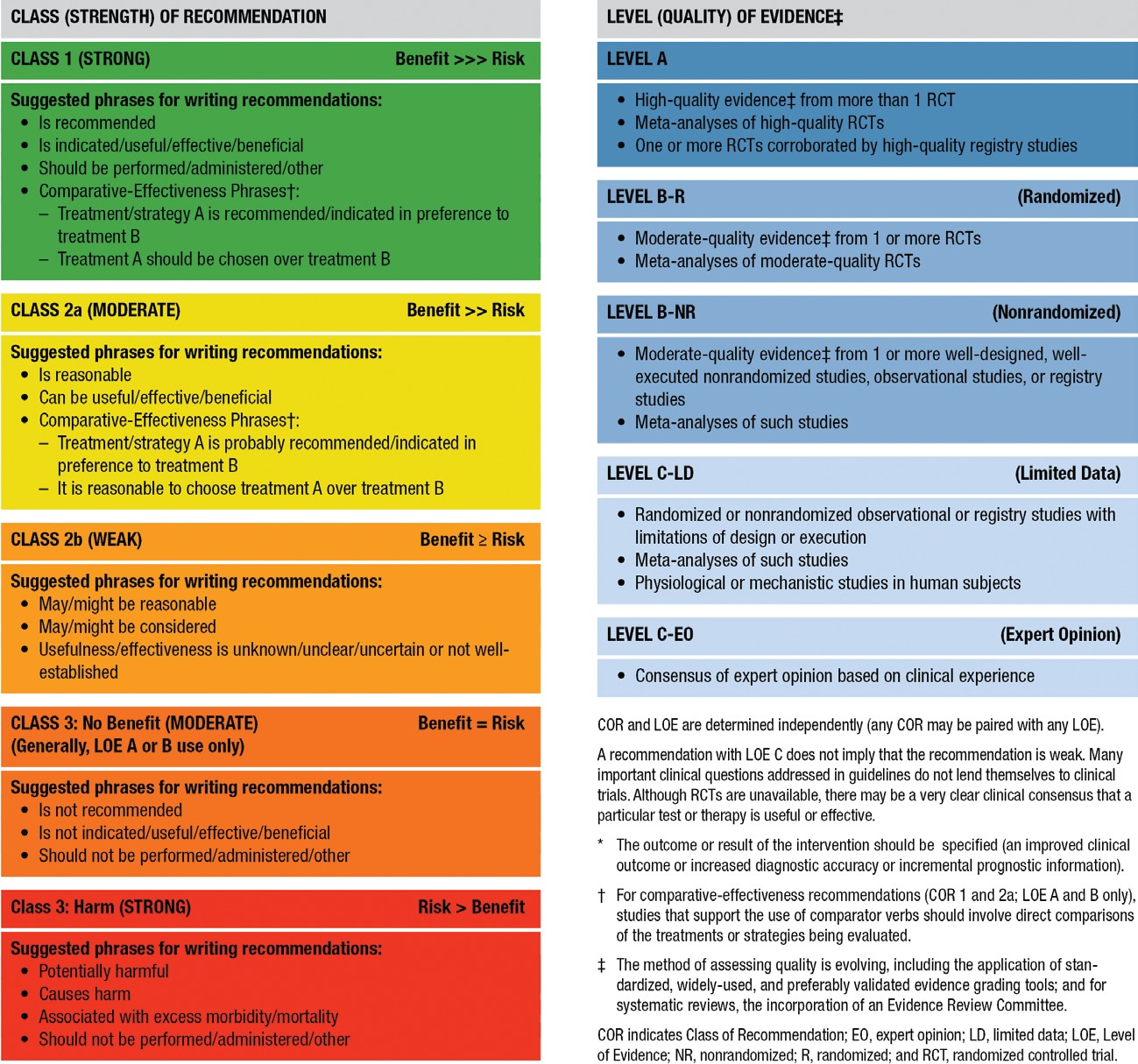
Class of Recommendation and Level of Evidence
As with all AHA guidelines, each recommendation in this focused update is assigned a Class of Recommendation (COR) on the basis of the strength of the evidence, alternative treatment options, and the effect on patients and society (Table). The Level of Evidence (LOE) is based on the quality, quantity, relevance, and consistency of the available evidence. For each recommendation, the writing group discussed and approved specific wording of recommendations and the COR and LOE assignments. In determining the COR, the writing group considered the LOE and other factors, including systems issues, economic factors, and ethical factors such as equity, acceptability, and feasibility. These evidence review methods, including specific criteria used to determine COR and LOE, are described more fully in “Part 2: Evidence Evaluation and Guidelines Development” of the 2020 guidelines.9 The writing group members had final authority over and formally approved these recommendations.
The overall certainty of the evidence base for neonatal resuscitation science is low. Funding and support for high-certainty clinical trials is a significant need in neonatal resuscitation. Of the 8 recommendations in this focused update, no recommendations are supported by Level A evidence (high-quality evidence from >1 randomized controlled trial [RCT], or ≥1 RCTs corroborated by high-quality registry studies). Five recommendations are supported by Level B-R (randomized) evidence (moderate evidence from ≥1 RCTs) and 1 by Level B-N (nonrandomized) evidence. Two recommendations are based on Level C evidence supported by limited data; no recommendations are based on Level C evidence derived from expert opinion. Likewise, the strength of recommendations is weaker than optimal: no Class 1 (strong) recommendations, 3 Class 2a (moderate) recommendations, 3 Class 2b (weak) recommendations, and 2 Class 3: No Benefit recommendations are included in these guidelines. There are no recommendations designated Class 3: Harm.
©2023 American Academy of Pediatrics and American Heart Association Inc
Table. Applying the American College of Cardiology/American Heart AssociationClass of Recommendation and Level of Evidence to Clinical Strategies, Interventions, Treatments, or Diagnostic Testing in Patient Care* (Up- dated May 2019)
Guideline Structure
These guidelines are organized into knowledge chunks, grouped into discrete modules of information on specific topics or management issues.9,10 Each modular knowledge chunk includes a table of recommendations that uses the standard AHA nomenclature of COR and LOE. Recommendations are presented in order of COR: most potential benefit (Class 1), followed by lesser certainty of benefit (Class 2), and finally potential for harm or no benefit (Class 3). Following the COR, recommendations are ordered by the certainty of supporting LOE: Level A (high-quality randomized controlled trials) to Level C-EO (expert opinion). A brief introduction puts the recommendations into context with important background information and overarching management or treatment concepts. Recommendation-specific text clarifies the rationale and key study data supporting the recommendations. Hyperlinked references facilitate quick access and review. All writing group members reviewed and approved the final manuscript.
©2023 American Academy of Pediatrics and American Heart Association Inc
Document Review and Approval
These guidelines were submitted for blinded peer review to 11 subject-matter experts nominated by the AHA and the AAP. Before appointment, all peer reviewers were required to disclose relationships with industry and any other conflicts of interest, and all disclosures were reviewed by AHA staff. Peer reviewer feedback was provided for guidelines in draft format and again in final format. All guidelines were reviewed and approved for publication by the AHA Science Advisory and Coordinating Committee, the AHA Executive Committee, and the AAP Executive Board. Comprehensive disclosure information for peer reviewers is listed in Appendix 2.
These recommendations augment the last full set of AHA recommendations for neonatal resuscitation made in 2020.7 All other recommendations and algorithms published in the 2020 guidelines remain the official recommendations of the AHA Emergency Cardiovascular Care Science Subcommittee and writing groups.
REFERENCES
-
- Gomersall J, Berber S, Middleton P, McDonald SJ, Niermeyer S, El-Naggar W, Davis PG, Schmolzer GM, Ovelman C, Soll RF, et al. Umbilical cord management at term and late preterm birth: a meta-analysis. Pediatrics. 2021;147:e2020015404. doi: 10.1542/peds.2020-015404
- Seidler AL, Gyte GML, Rabe H, Diaz-Rossello JL, Duley L, Aziz K, Testoni Costa-Nobre D, Davis PG, Schmolzer GM, Ovelman C, et al. Umbilical cord management for newborns <34 weeks’ gestation: a meta-analysis. Pediatrics. 2021;147:e20200576. doi: 10.1542/peds.2020-0576
- Trevisanuto D, Roehr CC, Davis PG, Schmölzer GM, Wyckoff MH, Liley HG, Rabi Y, Weiner GM. Devices for administering ventilation at birth: a systematic review. Pediatrics. 2021;148:e2021050174. doi: 10.1542/peds.2021-050174
- Yamada NK, McKinlay CJ, Quek BH, Schmölzer GM, Wyckoff MH, Liley HG, Rabi Y, Weiner GM. Supraglottic airways compared with face masks for neonatal resuscitation: a systematic review. Pediatrics. 2022;150:e2022056568. doi: 10.1542/peds.2022-056568
- Wyckoff MH, Singletary EM, Soar J, Olasveengen TM, Greif R, Liley HG, Zideman D, Bhanji F, Andersen LW, Avis SR, et al. 2021 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the Basic Life Support; Advanced Life Support; Neonatal Life Support; Education, Implementation, and Teams; First Aid Task Forces; and the COVID-19 Working Group. Circulation. 2022;145:e645–e721. doi: 10.1161/CIR.0000000000001017
- Wyckoff MH, Greif R, Morley PT, Ng K-C, Olasveengen TM, Singletary EM, Soar J, Cheng A, Drennan IR, Liley HG, et al. 2022 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Circulation. 2022;146:e483–e557. doi: 10.1161/CIR.0000000000001095
- Aziz K, Lee HC, Escobedo MB, Hoover AV, Kamath-Rayne BD, Kapadia VS, Magid DJ, Niermeyer S, Schmolzer GM, Szyld E, et al. Part 5: neonatal resuscitation: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142(16_suppl_2):S524–S550. doi: 10.1161/CIR.0000000000000902
- Wyckoff MH, Wyllie J, Aziz K, de Almeida MF, Fabres J, Fawke J, Guinsburg R, Hosono S, Isayama T, Kapadia VS, et al. Neonatal life support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2020;142:S185–S221. doi: 10.1161/CIR.0000000000000895
- Magid DJ, Aziz K, Cheng A, Hazinski MF, Hoover AV, Mahgoub M, Panchal AR, Sasson C, Topjian AA, Rodriguez AJ, et al. Part 2: evidence evaluation and guidelines development: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142:S358–S365. doi: 10.1161/CIR.0000000000000898
- Levine GN, O’Gara PT, Beckman JA, Al-Khatib SM, Birtcher KK, Cigarroa JE, de Las Fuentes L, Deswal A, Fleisher LA, Gentile F, et al. Recent innovations, modifications, and evolution of ACC/AHA clinical practice guidelines: an update for our constituencies: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e879–e886. doi: 10.1161/cir.0000000000000651
©2023 American Academy of Pediatrics and American Heart Association Inc
UMBILICAL CORD MANAGEMENT
Background
Management of the umbilical cord and placental transfusion at delivery remains an area of robust investigation. The volume of blood transferred from the placenta to the newborn infant and the effect of that transfusion vary on the basis of gestational age at delivery, mode of delivery, the time from delivery to cord clamping, any milking of the umbilical cord, and physiological status of the newborn infant.
Both the American College of Obstetrics and Gynecology and the AAP have produced guidelines about umbilical cord management.1,2 The most recent guidance from the AHA was published in 2020 and included all gestational ages and methods of placental transfusion.3 However, the developmental differences between preterm, late preterm, and term infants affect the outcomes of different cord management strategies, including the need for cardiorespiratory support in the delivery room, rate of moderate-to-severe hypoxic-ischemic encephalopathy, hematologic indices, need for admission to the neonatal intensive care unit, and use of therapeutic hypothermia. Because of these variations, ILCOR subsequently performed 2 different systematic reviews for cord management, 1 for late preterm and term infants4 and 1 for preterm infants.5 This focused update provides separate recommendations for these 2 distinct groups and relevant evidence published since those meta-analyses through September 2022.
| Recommendations for Term/Late Preterm Newborn Umbilical Cord Management | ||
| COR | LOE | Recommendations |
| 2a | B-R | 1. For term and late preterm newborn infants ≥34 weeks’ gestation who do not require resuscitation, delayed cord clamping (DCC) (≥30 seconds) can be beneficial when compared to early cord clamping (<30 seconds). |
| 2b | B-R | 2. For nonvigorous term and late preterm infants (35–42 weeks’ gestation), intact cord milking may be reasonable when compared to early cord clamping (<30 seconds). |
| 3: No
Benef it |
C-LD | 3. For term and late preterm newborn infants ≥34 weeks’ gestation who do not require resuscitation, intact cord milking is not known to be beneficial when compared to DCC (≥30 seconds). |
Recommendation-Specific Supportive Text
-
- Four RCTs (537 infants) found no difference in mortality between early and late cord clamping for term and late preterm infants.6–9 Low-certainty evidence from 15 studies (2641 infants) shows that DCC results in increased early hematologic indices (either hemoglobin or hematocrit) compared with early cord clamping.7,8,10–22
- One RCT including 1730 nonvigorous newborn infants limited to 35 to 42 weeks’ gestation (not including infants 34
©2023 American Academy of Pediatrics and American Heart Association Inc
weeks’ gestation) comparing intact umbilical cord milking with early cord clamping found no difference in the primary outcome of admission to the neonatal intensive care unit. However, differences in several secondary outcomes (including increased hemoglobin levels and a reduced need for cardiorespiratory support) make umbilical cord milking in this population a reasonable option.23 Additional studies would be helpful in further evaluating this intervention.
-
- There is no evidence available to support intact cord milking compared with DCC in vigorous term and late preterm infants.
| Recommendations for Preterm Newborn Umbilical Cord Management | ||
| COR | LOE | Recommendations |
| 2a | B-R | 1. For preterm newborn infants <34 weeks’ gestation who do not require resuscitation, delaying cord clamping (≥30 seconds) can be beneficial when compared to early cord clamping (<30 seconds). |
| 2b | B-R | 2. For preterm newborn infants between 28 and 34 weeks’ gestation who do not require resuscitation and in whom DCC cannot be performed, intact cord milking may be reasonable. |
| 3: No
Benef it |
B-R | 3. For preterm newborn infants <28 weeks’ gestation, intact cord milking is not recommended. |
Recommendation-Specific Supportive Text
- Sixteen RCTs (2988 infants) showed possible improvement in survival to discharge for infants receiving DCC compared with early cord clamping. DCC varied from 30 seconds to >2 minutes.24–39 Six studies (351 infants) showed that infants receiving DCC had decreased inotrope use in the first 24 hours.33,36–38,40,41 Infants receiving DCC had improved hematologic indices within 24 hours and 7 days,24–27,31–43 and received fewer red blood cell transfusions during admission.24,27,28,32,35,37–40,42–44
- Intact cord milking a.
Versus early cord clamping: In 11 trials (983 infants), infants receiving intact cord milking had higher hematologic indices in the first 24 hours.43,45–55 In 5 trials (439 infants), infants receiving intact cord milking received fewer inotropes in the first 24 hours.45–47,49,55 In infants 28 to 32 weeks’ gestation, 10 studies (889 infants) could not exclude benefit or harm of intact cord milking for severe intraventricular hemorrhage.43,45–47,49,51–53,55,56
b.
Versus DCC: A single trial including 292 preterm infants (28–31+6/7 weeks’ gestation) showed no increased risk of
severe intraventricular hemorrhage for umbilical cord milking compared with DCC.57
- In a single study of 182 infants born 23 to 27+6/7 weeks’ gestation not requiring resuscitation, severe intraventricular hemorrhage was significantly higher in those who received umbilical cord milking compared with DCC.57
©2023 American Academy of Pediatrics and American Heart Association Inc
REFERENCES
- American College of Obstetricians and Gynecologists’ Committee on Obstetric Practice. Delayed umbilical cord clamping after
birth: ACOG committee opinion, Number 814. Obstet Gynecol. 2020;136:e100–e106. doi: 10.1097/AOG.0000000000004167
- American Academy of Pediatrics. Delayed umbilical cord clamping after birth. Pediatrics. 2017;139:e2017095. doi: 10.1542/peds.2017-0957
- Aziz K, Lee HC, Escobedo MB, Hoover AV, Kamath-Rayne BD, Kapadia VS, Magid DJ, Niermeyer S, Schmolzer GM, Szyld E, et al. Part 5: neonatal resuscitation: 2020 American Heart Association Guidelines for Cardiopulmonary -Resuscitation and Emergency -Cardiovascular Care. Circulation. 2020;142(16_suppl_2):S524–S550. doi: 10.1161/CIR.0000000000000902
- Gomersall J, Berber S, Middleton P, McDonald SJ, Niermeyer S, El-Naggar W, Davis PG, Schmolzer GM, Ovelman C, Soll RF, et al. Umbilical cord management at term and late preterm birth: a meta-analysis. Pediatrics. 2021;147:e2020015404. doi: 10.1542/peds.2020-015404
- Seidler AL, Gyte GML, Rabe H, Diaz-Rossello JL, Duley L, Aziz K, Testoni Costa-Nobre D, Davis PG, Schmolzer GM, Ovelman C, et al. Umbilical cord management for newborns <34 weeks’ gestation: a meta-analysis. Pediatrics. 2021;147:e20200576. doi: 10.1542/peds.2020-0576
- Backes CH, Huang H, Cua CL, Garg V, Smith CV, Yin H, Galantowicz M, Bauer JA, Hoffman TM. Early versus delayed umbilical cord clamping in infants with congenital heart disease: a pilot, randomized, controlled trial. J Perinatol. 2015;35:826–831. doi: 10.1038/jp.2015.89
- Ceriani Cernadas JM, Carroli G, Pellegrini L, Otano L, Ferreira M, Ricci C, Casas O, Giordano D, Lardizabal J. The effect of timing of cord clamping on neonatal venous hematocrit values and clinical outcome at term: a randomized, controlled trial. Pediatrics. 2006;117:e779–e786. doi: 10.1542/peds.2005-1156
- Chopra A, Thakur A, Garg P, Kler N, Gujral K. Early versus delayed cord clamping in small for gestational age infants and iron stores at 3 months of age: a randomized controlled trial. BMC Pediatr. 2018;18:234. doi: 10.1186/s12887-018-1214-8
- Datta BV, Kumar A, Yadav R. A randomized controlled trial to evaluate the role of brief delay in cord clamping in preterm neonates (34–36 weeks) on short-term neurobehavioural outcome. J Trop Pediatr. 2017;63:418–424. doi: 10.1093/tropej/fmx004
- Al-Tawil MM, Abdel-Aal MR, Kaddah MA. A randomized controlled trial on delayed cord clamping and iron status at 3–5 months in term neonates held at the level of maternal pelvis. J Neonatal-Perinat Med. 2012;5:319–326. doi: 10.3233/npm-1263112
- Chaparro CM, Neufeld LM, Tena Alavez G, Eguia-Liz Cedillo R, Dewey KG. Effect of timing of umbilical cord clamping on iron status in Mexican infants: a randomised controlled trial. Lancet. 2006;367:1997–2004. doi: 10.1016/S0140-6736(06)68889-2
- Chen X, Li X, Chang Y, Li W, Cui H. Effect and safety of timing of cord clamping on neonatal hematocrit values and clinical outcomes in term infants: a randomized controlled trial. J Perinatol. 2018;38:251–257. doi: 10.1038/s41372-017-0001-y
- De Paco C, Herrera J, Garcia C, Corbalán S, Arteaga A, Pertegal M, Checa R, Prieto MT, Nieto A, Delgado JL. Effects of delayed cord clamping on the third stage of labour, maternal haematological parameters and acid-base status in fetuses at term. Eur J Obstet Gynecol Reprod Biol. 2016;207:153–156. doi: 10.1016/j.ejogrb.2016.10.031
- Emhamed MO, van Rheenen P, Brabin BJ. The early effects of delayed cord clamping in term infants born to Libyan mothers.
Trop Doct. 2004;34:218–222. doi: 10.1177/004947550403400410
- Fawzy AE-MA, Moustafa , El-Kassar AA, El-Kassar YS, Swelem MS, El-Agwany AS, Diab DA. Early versus delayed cord clamping of term births in Shatby Maternity University Hospital. Prog Obstet Ginecol. 2015;58:389–392. doi: 10.1016/j.pog.2015.05.001
- Jahazi A, Kordi M, Mirbehbahani NB, Mazloom SR. The effect of early and late umbilical cord clamping on neonatal hematocrit.
J Perinatol. 2008;28:523–525. doi: 10.1038/jp.2008.55
- Mohammad K, Tailakh S, Fram K, Creedy D. Effects of early umbilical cord clamping versus delayed clamping on maternal and neonatal outcomes: a Jordanian study. J Matern Fetal Neonatal Med. 2021;34:231–237. doi: 10.1080/14767058.2019.1602603
- Philip AG. Further observations on placental transfusion. Obstet Gynecol. 1973;42:334–343.
- Salari Z, Rezapour M, Khalili N. Late umbilical cord clamping, neonatal hematocrit and Apgar scores: a randomized controlled trial. J Neonatal Perinatal Med. 2014;7:287–291. doi: 10.3233/NPM-1463913
- Ultee CA, van der Deure J, Swart J, Lasham C, van Baar AL. Delayed cord clamping in preterm infants delivered at 34–36 weeks’
gestation: a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed. 2008;93:F20–F23. doi: 10.1136/adc.2006.100354
- Vural I, Ozdemir H, Teker G, Yoldemir T, Bilgen H, Ozek E. Delayed cord clamping in term large-for-gestational age infants: a prospective randomised study. J Paediatr Child Health. 2019;55:555–560. doi: 10.1111/jpc.14242
- Yadav AK, Upadhyay A, Gothwal S, Dubey K, Mandal U, Yadav CP. Comparison of three types of intervention to enhance placental redistribution in term newborns: randomized control trial. J Perinatol. 2015;35:720–724. doi: 10.1038/jp.2015.65
- Katheria AC, Clark E, Yoder B, Schmolzer GM, Yan Law BH, El-Naggar W, Rittenberg D, Sheth S, Mohamed MA, Martin C, et al. Umbilical cord milking in nonvigorous infants: a cluster-randomized crossover trial. Am J Obstet Gynecol. 2023;228:217.e1–217.e14. doi: 10.1016/j.ajog.2022.08.015
©2023 American Academy of Pediatrics and American Heart Association Inc
- Armanian AM, Tehrani HG, Ansari M, Ghaemi S. Is “delayed umbilical cord clamping” beneficial for premature newborns?. Int J Pediatr. 2017;5:4909–4918. doi: 10.22038/ijp.2016.7909
- Backes CH, Huang H, Iams JD, Bauer JA, Giannone PJ. Timing of umbilical cord clamping among infants born at 22 through 27
weeks’ gestation. J Perinatol. 2016;36:35–40. doi: 10.1038/jp.2015.117
- Baenziger O, Stolkin F, Keel M, von Siebenthal K, Fauchere JC, Das Kundu S, Dietz V, Bucher HU, Wolf M. The influence of the timing of cord clamping on postnatal cerebral oxygenation in preterm neonates: a randomized, controlled trial. Pediatrics. 2007;119:455–459. doi: 10.1542/peds.2006-2725
- Das B, Sundaram V, Kumar P, Mordi WT, Dhaliwal LK, Das R. Effect of placental transfusion on iron stores in moderately preterm neonates of 30–33 weeks gestation. Indian J Pediatr. 2018;85:172–178. doi: 10.1007/s12098-017-2490-2
- Duley L, Dorling J, Pushpa-Rajah A, Oddie SJ, Yoxall CW, Schoonakker B, Bradshaw L, Mitchell EJ, Fawke JA, Cord Pilot Trial Collaborative Group. Randomised trial of cord clamping and initial stabilisation at very preterm birth. Arch Dis Child Fetal Neonatal Ed. 2018;103:F6–F14. doi: 10.1136/archdischild-2016-312567
- Hofmeyr GJ, Bolton KD, Bowen DC, Govan JJ. Periventricular/intraventricular haemorrhage and umbilical cord clamping. Findings and hypothesis. S Afr Med J. 1988;73:104–106.
- Hofmeyr GJ, Gobetz L, Bex PJ, Van der Griendt M, Nikodem C, Skapinker R, Delahunt T. Periventricular/intraventricular hemorrhage following early and delayed umbilical cord clamping. A randomized controlled trial. Online J Curr Clin Trials. 1993;Doc No 110.
- Kinmond S, Aitchison TC, Holland BM, Jones JG, Turner TL, Wardrop CA. Umbilical cord clamping and preterm infants: a randomised trial. BMJ. 1993;306:172–175. doi: 10.1136/bmj.306.6871.172
- Kugelman A, Borenstein-Levin L, Riskin A, Chistyakov I, Ohel G, Gonen R, Bader D. Immediate versus delayed umbilical cord clamping in premature neonates born <35 weeks: a prospective, randomized, controlled study. Am J Perinatol. 2007;24:307–315. doi: 10.1055/s-2007-981434
- McDonnell M, Henderson-Smart DJ. Delayed umbilical cord clamping in preterm infants: a feasibility study. J Paediatr Child Health. 1997;33:308–310. doi: 10.1111/j.1440-1754.1997.tb01606.x
- Mercer JS, McGrath MM, Hensman A, Silver H, Oh W. Immediate and delayed cord clamping in infants born between 24 and 32 weeks: a pilot randomized controlled trial. J Perinatol. 2003;23:466–472. doi: 10.1038/sj.jp.7210970
- Mercer JS, Vohr BR, Erickson-Owens DA, Padbury JF, Oh W. Seven-month developmental outcomes of very low birth weight infants enrolled in a randomized controlled trial of delayed versus immediate cord clamping. J Perinatol. 2010;30:11–16. doi: 10.1038/jp.2009.170
- Oh W, Fanaroff AA, Carlo WA, Donovan EF, McDonald SA, Poole WK. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Effects of delayed cord clamping in very-low-birth-weight infants. J Perinatol. 2011;31(suppl 1):S68–S71. doi: 10.1038/jp.2010.186
- Rabe H, Wacker A, Hulskamp G, Hornig-Franz I, Schulze-Everding A, Harms E, Cirkel U, Louwen F, Witteler R, Schneider HP. A randomised controlled trial of delayed cord clamping in very low birth weight preterm infants. Eur J Pediatr. 2000;159:775–777. doi: 10.1007/pl00008345
- Ruangkit C, Bumrungphuet S, Panburana P, Khositseth A, Nuntnarumit P. A randomized controlled trial of immediate versus delayed umbilical cord clamping in multiple-birth infants born preterm. Neonatology. 2019;115:156–163. doi: 10.1159/000494132
- Tarnow-Mordi W, Morris J, Kirby A, Robledo K, Askie L, Brown R, Evans N, Finlayson S, Fogarty M, Gebski V, et al. Delayed versus immediate cord clamping in preterm infants. N Engl J Med. 2017;377:2445–2455. doi: 10.1056/NEJMoa1711281
- Dong XY, Sun XF, Li MM, Yu ZB, Han SP. Influence of delayed cord clamping on preterm infants with a gestational age of <32
weeks [in Chinese]. Zhongguo Dang Dai Er Ke Za Zhi. 2016;18:635–638. doi: 10.7499/j.issn.1008-8830.2016.07.013
- Gokmen Z, Ozkiraz S, Tarcan A, Kozanoglu I, Ozcimen EE, Ozbek N. Effects of delayed umbilical cord clamping on peripheral blood hematopoietic stem cells in premature neonates. J Perinat Med. 2011;39:323–329. doi: 10.1515/jpm.2011.021
- Dipak NK, Nanavat RN, Kabra NK, Srinivasan A, Ananthan A. Effect of delayed cord clamping on hematocrit, and thermal and hemodynamic stability in preterm neonates: a randomized controlled trial. Indian Pediatr. 2017;54:112–115. doi: 10.1007/s13312-017-1011-8
- Finn D, Ryan DH, Pavel A, O’Toole JM, Livingstone V, Boylan GB, Kenny LC, Dempsey EM. Clamping the umbilical cord in premature deliveries
(CUPiD): neuromonitoring in the immediate newborn period in a randomized, controlled trial of preterm infants born at <32
weeks of gestation. J Pediatr. 2019;208:121–126.e122. doi: 10.1016/j.jpeds.2018.12.039
- Rana A, Agarwal K, Ramji S, Gandhi G, Sahu L. Safety of delayed umbilical cord clamping in preterm neonates of less than 34 weeks of gestation: a randomized controlled trial. Obstet Gynecol Sci. 2018;61:655–661. doi: 10.5468/ogs.2018.61.6.655
- Elimian A, Goodman J, Escobedo M, Nightingale L, Knudtson E, Williams M. Immediate compared with delayed cord clamping in the preterm neonate: a randomized controlled trial. Obstet Gynecol. 2014;124:1075–1079. doi: 10.1097/AOG.0000000000000556
- El-Naggar W, Simpson D, Hussain A, Armson A, Dodds L, Warren A, Whyte R, McMillan D. Cord milking versus immediate clamping in preterm infants: a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed. 2019;104:F145–F150. doi: 10.1136/archdischild-2018-314757
©2023 American Academy of Pediatrics and American Heart Association Inc
- Hosono S, Mugishima H, Fujita H, Hosono A, Minato M, Okada T, Takahashi S, Harada K. Umbilical cord milking reduces the need for red cell transfusions and improves neonatal adaptation in infants born at less than 29 weeks’ gestation: a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed. 2008;93:F14–F19. doi: 10.1136/adc.2006.108902
- Katheria A, Blank D, Rich W, Finer N. Umbilical cord milking improves transition in premature infants at birth. PLoS One. 2014;9:e94085. doi: 10.1371/journal.pone.0094085
- Katheria AC, Leone TA, Woelkers D, Garey DM, Rich W, Finer NN. The effects of umbilical cord milking on hemodynamics and neonatal outcomes in premature neonates. J Pediatr. 2014;164:1045–1050.e1. doi: 10.1016/j.jpeds.2014.01.024
- Kilicdag H, Gulcan H, Hanta D, Torer B, Gokmen Z, Ozdemir SI, Antmen BA. Is umbilical cord milking always an advantage? J Matern Fetal Neonatal Med. 2016;29:615–618. doi: 10.3109/14767058.2015.1012067
- Li J, Yu B, Wang W, Luo D, Dai QL, Gan XQ. Does intact umbilical cord milking increase infection rates in preterm infants with premature prolonged rupture of membranes?. J Matern Fetal Neonatal Med. 2020;33:184–190. doi: 10.1080/14767058.2018.1487947
- March MI, Hacker MR, Parson AW, Modest AM, de Veciana M. The effects of umbilical cord milking in extremely preterm infants: a randomized controlled trial. J Perinatol. 2013;33:763–767. doi: 10.1038/jp.2013.70
- Mercer JS, Erickson-Owens DA, Vohr BR, Tucker RJ, Parker AB, Oh W, Padbury JF. Effects of placental transfusion on neonatal and 18 month outcomes in preterm infants: a randomized controlled trial. J Pediatr. 2016;168:50–55.e51. doi: 10.1016/j.jpeds.2015.09.068
- Silahli M, Duman E, Gokmen Z, Toprak E, Gokdemir M, Ecevit A. The relationship between placental transfusion, and thymic size and neonatal morbidities in premature infants: a randomized control trial. J Pakistan Med Assoc. 2018;68:1560–1565.
- Song SY, Kim Y, Kang BH, Yoo HJ, Lee M. Safety of umbilical cord milking in very preterm neonates: a randomized controlled study. Obstet Gynecol Sci. 2017;60:527–534. doi: 10.5468/ogs.2017.60.6.527
- Alan S, Arsan S, Okulu E, Akin IM, Kilic A, Taskin S, Cetinkaya E, Erdeve O, Atasay B. Effects of umbilical cord milking on the need for packed red blood cell transfusions and early neonatal hemodynamic adaptation in preterm infants born ≤1500 g: a prospective, randomized, controlled trial. J Pediatr Hematol Oncol. 2014;36:e493–e498. doi: 10.1097/MPH.0000000000000143
- Katheria A, Reister F, Essers J, Mendler M, Hummler H, Subramaniam A, Carlo W, Tita A, Truong G, Davis-Nelson S, et al. Association of umbilical cord milking vs delayed umbilical cord clamping with death or severe intraventricular hemorrhage among preterm infants. JAMA. 2019;322:1877–1886. doi: 10.1001/jama.2019.16004
VENTILATORY SUPPORT AFTER BIRTH: DEVICES AND INTERFACES TO ADMINISTER PPV
Background
The 2020 AHA guidelines provided recommendations for when and how to provide PPV, including guidance for
-inflation pressures, the use of positive end-expiratory pressure, ventilation rate, and inspiratory time.1 The recommendations provided in this focused update discuss devices to deliver PPV, and the choice between a face mask and a supraglottic airway as the interface used for PPV.
Several devices are available to administer PPV, including self-inflating bags, flow-inflating bags, and T-piece resuscitators. The choice of PPV device depends on factors reflecting the context at a birthing site: the number of births, the case mix, availability of a compressed gas source, familiarity with the different devices, amount of training required to use each device, and device cost. Because both T-piece resuscitators and flow-inflating bags require a compressed gas source to function, a self-inflating bag should be available as a backup in the event of compressed gas failure when using either of these devices.
Available interfaces for PPV delivery include face masks, nasal prongs, and supraglottic airways. This focused update specifically addresses the choice between face masks and supraglottic airways as the primary interface during PPV.
©2023 American Academy of Pediatrics and American Heart Association Inc
| Recommendations for Devices Used to Administer PPV for Newborn Infants | ||
| COR | LOE | Recommendations |
| 2a | B-NR | 1. It can be beneficial to use a T-piece resuscitator instead of a self-inflating bag, with or without a positive
end-expiratory pressure valve, for administering positive-pressure ventilation to newborn infants, particularly for preterm infants. |
Recommendation-Specific Supportive Text
-
- A meta-analysis of 4 RCTs (1247 term and preterm infants) found that resuscitation with a T-piece resuscitator compared with a self-inflating bag reduced the duration of PPV and decreased risk of bronchopulmonary dysplasia.2 Although subgroup analyses by gestational age were not feasible in this meta-analysis, bronchopulmonary dysplasia is an outcome that affects preterm infants, and the use of a T-piece resuscitator may present the greatest benefit to preterm infants. The systematic review did not identify any studies that evaluated the use of flow-inflating bags.2
| Recommendation for Interfaces Used to Administer PPV for Newborn Infants | ||
| COR | LOE | Recommendation |
| 2b | C-LD | 1. It may be reasonable to use a supraglottic airway as the primary interface to administer PPV instead of a face mask for newborn infants delivered at
≥34 0/7 weeks’ gestation. |
Recommendation-Specific Supportive Text
1. A meta-analysis of 6 RCTs (1823 infants delivered at ≥34 0/7 weeks’ gestation) found that use of a supraglottic airway decreased the probability of failure to improve with the assigned device, and the rate of endotracheal intubation in the delivery room.3 Failure to improve with the assigned device was a pragmatic outcome chosen to assess whether primary use of the supraglottic airway or face mask to provide PPV led to improvement of neonates undergoing resuscitation after birth. The duration of PPV and time until heart rate reached >100/min were also shorter with the supraglottic airway.
©2023 American Academy of Pediatrics and American Heart Association Inc
Based on available evidence, this recommendation is limited to newborn infants ≥34 0/7 weeks’ gestation. All studies included in this meta-analysis were performed in lower-resourced settings. No studies have compared face masks with supraglottic devices for initiating PPV during neonatal resuscitation in high-resourced settings. As a result, the effect size reported in this meta-analysis may not be generalizable to settings with greater availability of health care practitioners with advanced skills and highly trained neonatal resuscitation teams.
REFERENCES
- Aziz K, Lee HC, Escobedo MB, Hoover AV, Kamath-Rayne BD, Kapadia VS, Magid DJ, Niermeyer S, Schmolzer GM, Szyld E, et al. Part 5: neonatal resuscitation: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142(16_suppl_2):S524–S550. doi: 10.1161/CIR.0000000000000902
- Trevisanuto D, Roehr CC, Davis PG, Schmölzer GM, Wyckoff MH, Liley HG, Rabi Y, Weiner GM. Devices for administering ventilation at birth: a systematic review. Pediatrics. 2021;148:e2021050174, doi: 10.1542/peds.2021-050174
- Yamada NK, McKinlay CJ, Quek BH, Schmölzer GM, Wyckoff MH, Liley HG, Rabi Y, Weiner GM. Supraglottic airways compared with face masks for neonatal resuscitation: a systematic review. Pediatrics. 2022;150:e2022056568. doi: 10.1542/peds.2022-056568
KNOWLEDGE GAPS AND PRIORITIES OF RESEARCH ACKNOWLEDGMENTS
This focused update is limited to a review of the science on umbilical cord management in term, late preterm, and preterm newborn infants and on the devices and interfaces used for administering PPV during resuscitation of newborn infants. The topics in the knowledge chunks of this update contain additional questions and practices for which evidence was weak, uncertain, or absent. In addition, the following knowledge gaps require further research:
Umbilical Cord Management
-
- Optimal management of the umbilical cord in term, late preterm, and preterm infants who require resuscitation at
delivery
-
- Longer-term outcome data, such as anemia during infancy and neurodevelopmental outcomes, for all umbilical cord management strategies
Devices for Administering PPV
-
- Cost-effectiveness of a T-piece resuscitator compared with a self-inflating bag
- The effect of a self-inflating bag with a positive end-expiratory pressure valve on outcomes in preterm newborn infants
- Comparison of either a T-piece resuscitator or a self-inflating bag with a flow-inflating bag for administering PPV
- Comparison of clinical outcomes by gestational age for any PPV device
Interfaces for Administering PPV
-
- Comparison of supraglottic airway devices and face masks as the primary interface for PPV in high-resourced settings
- The amount and type of training required for successful supraglottic airway insertion and the potential for skill decay
- The utility of supraglottic airway devices for suctioning secretions from the airway
- The efficacy of a supraglottic airway during advanced neonatal resuscitation requiring chest compressions or the
delivery of intratracheal medications
©2023 American Academy of Pediatrics and American Heart Association Inc
ARTICLE INFORMATION
The American Heart Association and the American Academy of Pediatrics make every effort to avoid any actual or potential conflicts of interest that may arise as a result of an outside relationship or a personal, professional, or business interest of a member of the writing panel. Specifically, all members of the writing group are required to complete and submit a Disclosure Questionnaire showing all such relationships that might be perceived as real or potential conflicts of interest.
This focused update was approved by the American Heart Association Science Advisory and Coordinating Committee on July 15, 2023; the American Heart Association Executive Committee on August 4, 2023; and the American Academy of Pediatrics on July 6, 2023.
This article has been copublished in Circulation.
The expert peer review of AHA-commissioned documents (eg, scientific statements, clinical practice guidelines, systematic reviews) is conducted by the AHA Office of Science Operations. For more on AHA statements and guidelines development, visit https://professional.heart.org/statements. Select the “Guidelines & Statements” drop-down menu, then click “Publication Development.”
Disclosures
Appendix 1. Writing Group Disclosures
| Writing group member | Employment | Research grant | Other research support | Speakers’ bureau/honora ria | Expert witness | Ownership interest | Consultant/ advisory board | Other |
| Henry C. Lee | University of California San Diego | None | None | None | None | None | None | None |
| Edgardo Szyld | Indiana University | None | None | None | None | None | None | None |
| Emer Finan | Mount Sinai Hospital; University of Toronto | None | None | None | None | None | None | None |
| Jessica L. Illuzzi | Yale School of Medicine | None | None | None | None | None | None | None |
| Beena D. Kamath-Rayne | American Academy of Pediatrics | None | None | None | None | None | None | Cerebral Palsy Alliance Research Foundation* |
| Vishal S. Kapadia | UT Southwestern | NIH†
Masimo Corporation† |
None | None | None | None | None | None |
| Susan Niermeyer | University of Colorado | NIH* | None | None | None | None | None | None |
| Georg M. Schmölzer | University of Alberta | CIHR Grant† CIHR Grant† | None | None | None | None | None | None |
| Marya L. Strand | Akron Children’s
Hospital |
None | None | None | None | None | None | None |
| Gary M. Weiner | University of Michigan | None | None | None | None | None | None | None |
| Amanda Williams | Cedars Sinai | None | None | None | None | None | None | None |
| Myra H. Wyckoff | UT Southwestern | None | None | None | None | None | None | None |
| Nicole K. Yamada | Stanford University | AHRQ†; AHRQ* | None | None | None | None | None | None |
This table represents the relationships of writing group members that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all members of the writing group are required to complete and submit. A relationship is considered to be “significant” if (a) the person receives $5000 or more during any 12-month period, or 5% or more of the person’s gross income; or (b) the person owns 5% or more of the voting stock or share of the entity, or owns $5000 or more of the fair market value of the entity. A relationship is considered to be “modest” if it is less than “significant” under the preceding definition.
*Modest.
†Significant.
©2023 American Academy of Pediatrics and American Heart Association Inc
Appendix 2. Reviewer Disclosures
| Reviewer | Employment | Research grant | Other research support | Speakers’ bureau/honora ria | Expert witness | Ownership interest | Consultant/ advisory board | Other |
| Ryan Alanzalon | Kaiser Permanente | None | None | None | None | None | None | None |
| Rakhi G. Basuray | The Ohio State University, Nationwide Children’s Hospital | None | None | None | None | None | None | None |
| Justin Goldstein | Beth Israel Deaconess Medical Center | None | None | None | None | None | None | None |
| Arun Gupta | Lucile Packard Children’s Hospital at Stanford University | None | None | None | None | None | None | None |
| Lia Lowrie | St. Louis University School of Medicine | None | None | None | None | None | None | None |
| Allison Markowsky | Children’s National
Hospital |
None | None | None | None | None | None | None |
| Saurabhkumar
C. Patel |
University of Illinois Chicago | None | None | None | None | None | None | None |
| Betsy Peterson | SOAPM | None | None | None | None | None | None | None |
| Clara Song | Kaiser Permanente | None | None | None | None | None | None | None |
| Michael R. Stenger | The Ohio State
-University |
None | None | None | None | None | None | None |
| Muhammad Waseem | Lincoln Medical Center | None | None | None | None | None | None | None |
This table represents the relationships of reviewers that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all reviewers are required to complete and submit. A relationship is considered to be “significant” if (a) the person receives $5000 or more during any 12-month period, or 5% or more of the person’s gross income; or (b) the person owns 5% or more of the voting stock or share of the entity, or owns $5000 or more of the fair market value of the entity. A relationship is considered to be “modest” if it is less than “significant” under the preceding definition.
©2023 American Academy of Pediatrics and American Heart Association Inc
Để lại một bình luận